
Sponsored by: American Heart Association

Applications for American Heart Association’s accelerator program are open now through June 28th. The EmPOWERED to Serve Business Accelerator offers selected founders six weeks of rigorous coaching and training around business model and branding, plus non-equity grants totaling $75,000.
Who should apply?
The accelerator is focused on empowering a diverse pool of health equity-focused founders. If you’re a founder of a nonprofit or pre-seed, seed, or series A startup focused on health equity, SDOH, or related focus areas, consider applying. Qualification and submission details are available here.
Register for the info session this week Tues, June 4 to learn more.
If you're interested in sponsoring the newsletter, let us know here.
NEWS
CVS is seeking investors to finance Oak Street clinic growth
Bloomberg reported last week that CVS is reaching out to private equity firms to explore forming a joint venture that would finance new clinic growth. The report notes that CVS is considering a similar structure to the joint venture that Humana and Welsh Carson created to finance Humana clinic growth.
✍ Going Deeper
It’s not exactly a surprise to hear that CVS is revisiting this approach to financing the initial losses of new Oak Street clinics given the financial pressures they’re facing for over the next few years.
A JV-like this is a potential win-win for both CVS and an investor, if that investor can get comfortable with Oak Street’s ability to consistently perform on its J-curve. If it does, the structure providers the investor with a relatively de-risked return on investment, and CVS gets the growth without the profitability hit.
At an investor presentation this week, CVS was quick to remind investors that Oak Street’s business is still performing as expected.
CVS’s CFO also noted that CVS has shared with investors since the acquisition that CVS might pursue alternative financing strategies for Oak Street clinic growth. Here’s a quote from CVS’s Q1 2023 earnings call about a year ago, just after the Oak Street acquisition closed:
For Oak Street, the early closing will allow us to explore alternative growth vehicles that allow us to accelerate clinic growth and mitigate dilution and, very importantly, begin this work well in advance of 2024….
…as we've discussed, though, there are vehicles and models where we could see kind of both accelerating the clinic growth and better managing the dilutive impact of that clinic growth. And now that we're closed, and we're closed well in advance of '24, I think one of the opportunities we have is to explore and potentially execute on those in time to have an impact on 2024.
The most interesting part of that quote from a year ago is the repeated emphasis on the fact that they planned to pursue a financing deal before 2024. Yet here we are almost halfway through 2024 without a deal done.
Why wait until now if you’re CVS leadership? Did they run a process last year, not like the potential terms they were seeing, and decide not to pursue a deal at that time? That seems like the most plausible outcome to me at least. If that’s the case, given the growing headwinds MA is facing over the past year, I can’t imagine CVS is getting better terms on a potential transaction today.
If you’re a PE shop — or any financial entity with the type of capital to fund a deal like this — I have to imagine that you’re viewing this deal as significantly riskier than the Humana deal given cash flow pressures over the next few years in the MA environment.
This all probably speaks to the level of EPS pressure that CVS is feeling at the moment in MA to cause CVS to revisit this structure as a potential growth strategy. If a deal does get done, it’ll be interesting to see what sort of terms CVS is able to get.
📖 Read More
Our review of the Oak Street / CVS merger transaction from Feb 2023
CVS & Oak Street’s merger slides presented to investors.
DATA
The strategic rationale for health systems adopting VBC
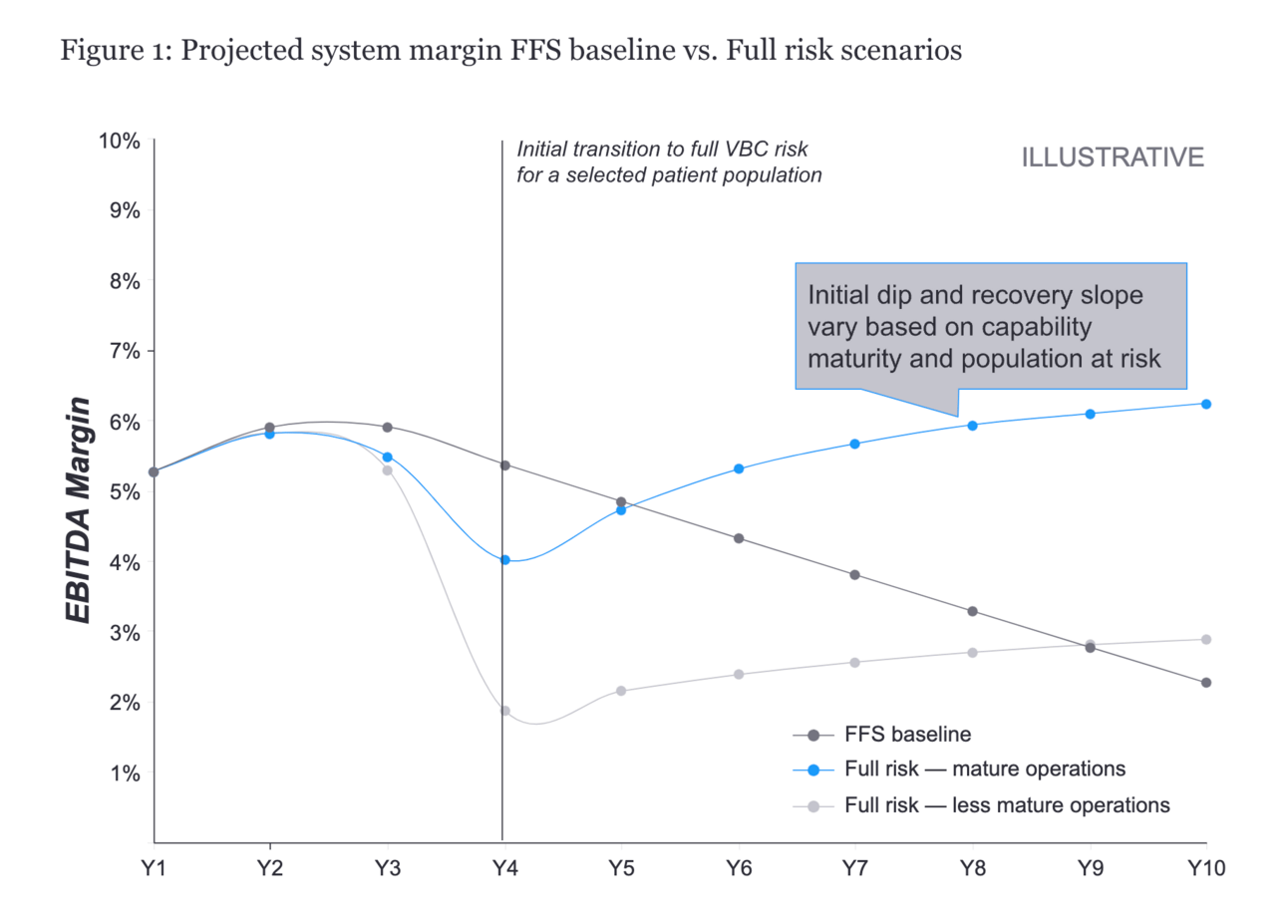
EY-Parthenon highlights the potential upside and downside for health system profitability in adopting risk-based contracts. The article highlights five capabilities that systems should invest in to succeed when moving to VBC: 1. growing attributed patients; 2. risk coding; 3. site of care management; 4. control OpEx; 5. physician alignment.
The chart above provides a nice visual of the potential EBITDA margin impact for health systems over the next decade. But if you listen to recent HCA and Tenet investor presentations, it certainly doesn’t sound like a given that the FFS baseline is going to shrink as the chart suggests.
The title of the article here is that VBC can boost health system revenue, and I actually think that’s incorrect. VBC can boost profitability for health system, but revenue should either decrease (or increase at a slower rate). This might seem like a minor nuance, but I actually think it’s one of the biggest challenges for health systems in adopting VBC. A health system Board and leadership team needs to have a lot of conviction in VBC if you believe the chart above. For the first few years of transition into VBC, revenue growth slows while profitability tanks in year 4, before potentially rebounding. You can understand why many health system Boards would be reluctant to pursue this approach.
Other news from the week:
Sound Physicians, a multi-specialty group with 4,000 clinicians practicing in 400+ hospitals across the country, restructured its debt and received $120 million in new capital. The debt restructuring had been in the works for some time and signals confidence from investors in Sounds’ long-term strategy.
The WSJ wrote a great report highlighting how 32BJ, a large union in the Northeast, attempted to kick NewYork-Presbyterian out of its insurance network while switching carriers from Elevance to Aetna. NewYork-Presbyterian demanded a $25 million payment in order to agree to be moved out of network.
Medicaid insurance stocks dropped this week as Centene and UnitedHealth told investors that they’re seeing pressure on Medicaid performance. Centene attributed this to a higher acuity population that remains on Medicaid after the redetermination process.
Minnesota passed legislation blocking for-profit insurance companies from participating in the state’s Medicaid program. UnitedHealth is the only for-profit insurer operating in the Medicaid program in Minnesota.
Dollar General and DocGo announced they are ending the mobile clinic pilot. No details were shared on the reasoning, but it’s not hard to imagine that Dollar General saw similar challenges to other retailers. The pilot was launched at three stores in Tennessee back in early 2023.
Clover Health announced its new SaaS platform product this week, called Counterpart Health. Clover shared at an investor conference that it intends to price the product as a PMPM and eventually get into capturing shared savings. The Counterpart website lists six client logos: a cardiology practice in NJ, a primary care practice in NJ, a primary care practice in TX and GA, a virtual primary care startup, Clover, and Duke’s ACO in NC.
Tempus AI publicly filed its S-1, kickstarting the IPO process.
Two Senate Committees, the Finance Committee and the HELP Committee, sent a letter to MultiPlan requesting a briefing on the recent New York Times article investigating MultiPlan’s pricing practices.
Centivo, an insurance plan for self-funded employers, acquired primary care startup Eden Health. Centivo had raised $100 million and worked with over 100 employers at the time of its Series C in 2021. After the acquisition, Centivo will have a combined 160 employer customers. It appears that Eden Health will be powering Centivo’s virtual care offering moving forward, as the press release doesn’t mention what will come of Eden’s six existing bricks-and-mortar practices.
Press Ganey refinanced its debt, replacing the debt with $1 billion in preferred equity that can be repurchased if Press Gainey goes public in the next 18 months.
Karoo Health, a VBC enabler for cardiology, partnered with Heartbeat Health, a virtual cardiology provider. It’s interesting to see in the press release that Karoo Health is bringing the model of care to the combined entity. I’d have thought that would be the other way around (meaning the docs would bring the model of care).
Blue Cross Blue Shield Association shared data from ~170,000 GLP-1 prescriptions finding that 30% of patients discontinued the medication within a month and almost 60% discontinued use before seeing a clinically meaningful health benefit.
Notable funding announcements:
Tuesday Health, a value-based model for end-of-life care, raised $60 million. The funding comes from Valtrius, Blue Venture Fund, CareSource (Ohio’s largest Medicaid plan), and Mass General Brigham Ventures.
Boulder Care, an addiction treatment care model targeting Medicaid populations, raised $35 million.
Atropos Health, a real-world clinical evidence platform, raised $33 million. Atropos has an interesting use case leveraging real-world data for clinicians to make clinical decisions at the point of care, and it appears from the press release that they’re finding traction in VBC models and the oncology space.
Wayspring, a VBC model for substance use disorder, raised funding from CVS Ventures.
SamaCare, a prior auth platform for specialty pharma, raised $17 million.
Plentful raised $17 million to use AI to automate pharmacy workflows.
CVS Ventures and Echo Health Ventures announced they participated in ThymeCare, an oncology care model, announced it added CVS Ventures and Echo Health Ventures to its previously announced funding round.
Oncovery Care (formerly Vivorcare), a cancer survivorship model, raised $4.5 million.
Superpower raised $4 million for a preventative care platform focused on longevity.
Good reads from the broader community:
The Promise and Challenge of Value-Based Payment by Daniel Shenfeld, Amol Navathe, and Ezekiel Emanuel
A quick read looking at the complexities of implementing VBC programs and suggesting that CMS make more data and analytics tools available.
The Doctor in the Corporation by Sachin Jain.
This is an interesting perspective on the tensions that providers have within organizations. As a provider, they have one set of obligations to patients. As a corporate leader, they have another set of commitments to corporate shareholders.
More from Health Tech Nerds
Exclusive to premium subscribers
The Library: Exploring Medical Costs in McAllen, TX. Revisiting Atul Gawande’s New Yorker report on ballooning health care spending in a small town in Texas and subsequent efforts to rein in spending.
Community Brain Trust Highlighting the past week’s most helpful conversations from the HTN Community including: Drata vs Vanta, an MSO for speech pathologists, drug savings cards and prior auths, and more
Featured Jobs
Director of Strategic Growth at N1 Health, an applied AI platform. Learn more.
Chief of Staff to CEO at Tomorrow Health, a home health technology platform. Learn more.
Director, Product Marketing at Rightway, a PBM. Learn more.
Director, US Government Strategy & Affairs at Vanta, a security and compliance platform. Learn more.
Manager, Business & Strategy at National Council for Mental Wellbeing, an advocacy organization for mental health and substance use care providers. Learn more.
Contact us to feature roles in our newsletter.
