This newsletter is sponsored by Stellar Health
Stellar Health helps health systems and large provider networks address a common problem: getting affiliate practices to perform various tasks and perform in VBC contracts. Think the ability to prompt, track and pay for day-to-day granular VBC activities such as (1) scheduling visits with high-risk patients (2) appropriately managing chronic conditions and (3) completing screenings or uploading results. There is often a lack of visibility and communication due to different EMRs and workflows, and Stellar can help drive workflow alignment across affiliate practices.
Stellar’s platform offers a dynamic, customizable value-based fee schedule for care teams. This creates real time earnings opportunities for care teams while minimizing the administrative time it takes to be successful in value based care contracts.
For more information on Stellar Health, visit www.stellar.health
News:
Kaiser acquires Geisinger and moves it under Risant Health, a new VBC platform for health systems
The big news of the week was this deal between Kaiser and Geisinger, and the creation of a new nonprofit, Risant. Risant will be a new value-based care platform that will seek to acquire another 4 to 5 health systems like Geisinger and form a national network of health systems in VBC contracts. Risant will attempt to get to $30 billion of revenue over the next five years. It all sounds really nice, but to be honest I’m not sure I have any clue what Risant will be doing here. It reads like Risant will act on behalf of Geisinger and five other massive health systems to manage VBC payor contracts and encourage the systems to adopt the same set of value-based care activities. Kaiser’s own struggles expanding the model outside California highlights the Sisyphean nature of the task at hand.
In many ways the move seems like a reaction to the moves the payors have been making in terms of building national platforms. The thesis of these platforms like UHG and CVS has been to leverage VBC contracts to steer utilization away from hospitals and reap the financial rewards. So it makes sense that health systems would band together in a defensive move to create their own national platform in response to this existential threat. There is safety in scale here, and so it’ll be fascinating to see who the next health systems are that sign up for the Risant platform (there were some good guesses in Slack this week). Link / Slack (h/t Andrew Byrk)
Bright is exploring the sale of Brand New Day and Central Health Plan
Brand New Day and Central Health plan were two key acquisitions Bright made to grow into the Medicare Advantage market in California. Bright acquired Brand New Day in early 2020 and Central Health Plan in early 2021. The continued slow drip of terrible news for Bright is exhausting to watch as an outsider, so I can only imagine what it feels like on the inside of the org right now. This news in particular seems like it might be the death knell for Bright.
Bright originally had until the end of April to raise additional capital or default on debt covenants and go bankrupt. The news this week included an extension of that period until the end of June, so Bright will have until then to sell these businesses and bring in more capital. It would appear that Bright has exhausted all other potential options to raise capital, which means that Bright’s inside investors are no longer putting more money in and leaves Bright in a really bad spot. It has run out of time, and the only way to avoid bankruptcy is to sell off a key asset for the business. Adding insult to injury, it would seem unlikely Bright will be able to sell those MA plans for anything near what they paid for them at the height of the market a few years ago, particularly given the headwinds facing MA rates over the coming years. It will be very interesting to see if a strategic or financial buyer emerges here, and who that buyer is.
Bright apparently will attempt to chart a path forward purely as a VBC primary care business, although you have to wonder if they just seek a buyer for those assets as well and call it a day. The press release itself hints this might be turning into a fire sale - it was curious to see the press release include a prominent quote from the lead independent director Manny Kadre articulating that the Board decided to sell the MA business. Why choose to quote Kadre, who is probably the least qualified board member to oversee a sale process of an MA business given he has no background in healthcare? How is Bob Sheehy - the current Board Chair, founding CEO, and former UHC CEO - not the person quoted there? It almost feels like Kadre has been tapped as the person to turn off the lights.
Humana earnings feature solid MA growth
As I mentioned in the Slack thread this week, Humana seemed pretty pleased with the benefits it is reaping from re-focusing on growth in Medicare Advantage. It saw solid membership growth in Open Enrollment and its attempts to shore up member acquisition channels appears to have worked. During the earnings call, Humana mentioned that this year it took 50% of new members from other carriers, up from 30% of new members who historically switched plans. Humana expects to be able to maintain this 50% rate moving forward. It was also interesting to hear that Humana only ever expects Centerwell clinics to be seeing below 5% of Humana members in any given market. This number appears to be playing out this year, as Centerwell business grew by 17k members while Humana’s non D-SNP membership grew by 474k, which would seem to imply that Humana has gotten at most 4% (17/474) of new members into a Centerwell clinic. That seems surprisingly low given the emphasis here. It’s also worth noting another question about whether the negative impacts of declining MA rates will be passed along to VBC providers, which will be something to keep an eye on.
Amazon’s brand of fitness devices, Halo, was shut down
The siren song of the wearables market strikes again, as Amazon was unable to make this business work after launching it only a few years ago. This business idea seems like catnip for tech execs who are the early adopters for tech like this and love the idea of capturing more data about their health. Yet time and time again, these initiatives fail to cross the chasm into the mainstream audience.
Opinions
Politico discusses the financial impact of a potential new Medicare benefit allowing for home health workers
While the new benefit is being pushed as a potential cost saving lever for Medicare, this article highlights some questions health economists have about whether that will actually materialize. Much of the discussion here is about whether this program will actually decrease costs for Medicare, or whether it will actually end up increasing costs. It seems like the safe bet is always that things will end up increasing costs in healthcare, but this is also one of those initiatives where we find ourselves wondering if that’s really such a bad thing. Clearly we have a problem with runaway healthcare costs in this country, but we’re hard pressed to understand how providing more resources for home health support is a bad thing.
A STAT interview highlights how a Nebraska hospital is doing well financially
Bob Herman conducted a fascinating interview with the CEO of a hospital in rural Nebraska that has a near monopoly on acute care delivery in the area. The hospital has done well financially through the pandemic, and despite staffing issues, volumes are up. It touches on some of the challenges they have in moving patients to post acute care and how Medicare Advantage is exacerbating some of those issues. It’s worth checking out as a counter-example to the broader narrative that hospitals, particularly those in rural environments, are doing poorly across the board. This one seems to be doing quite well.
A regulatory change sparks a hospital boom in Florida
It’s pretty wild to read this report in the context of the broader sense of the industry that hospitals are struggling mightily. In an affluent suburb of Tampa, two hospitals have opened within a two mile radius in the past few years, and another one is on the way. Since Florida changed its Certificate of Need (CON) process in 2019, 65 new hospitals have been planned in the state between 2020 - 2022. Not surprisingly, it appears these tend to be going in relatively affluent areas with commercial populations versus rural areas. It certainly invites lots of questions about how sustainable this all is, and how we collectively allocate scarce resources across the population. Having three different health systems building hospitals within two miles in Tampa sure doesn’t seem like it serves any purpose other than helping systems maintain the status quo in terms of commercial market share while jacking up prices to cover off on the costs of building these new buildings. But hey, BayCare’s new 86 bed hospital there does let patients use Alexa to dim the lights or play music in their rooms, so ya know, innovation for the win.
Commonwealth Fund highlights the challenges of Medicaid work requirements
The article does a nice job briefly articulating the impact of work requirements and some of the practical challenges with how federal funding might be clawed back long after it is doled out by the state.
Data
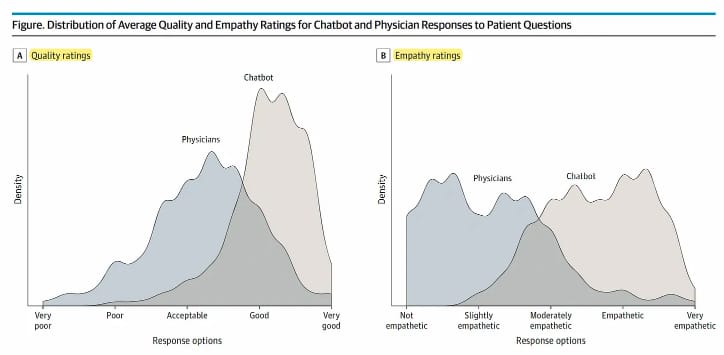
A new JAMA study suggests ChatGPT responds to questions from patients with higher quality answers and more empathy than providers
This is a wild study looking at how physicians and ChatGPT responded to questions from patients in a reddit channel. Three health care professionals reviewed the responses from each and found that ChatGPT had significantly higher rates across both quality and empathy. There are so many dimensions to this that boggle my mind. Obviously, there a lot of questions yet to be answered about ChatGPT, but, woah.
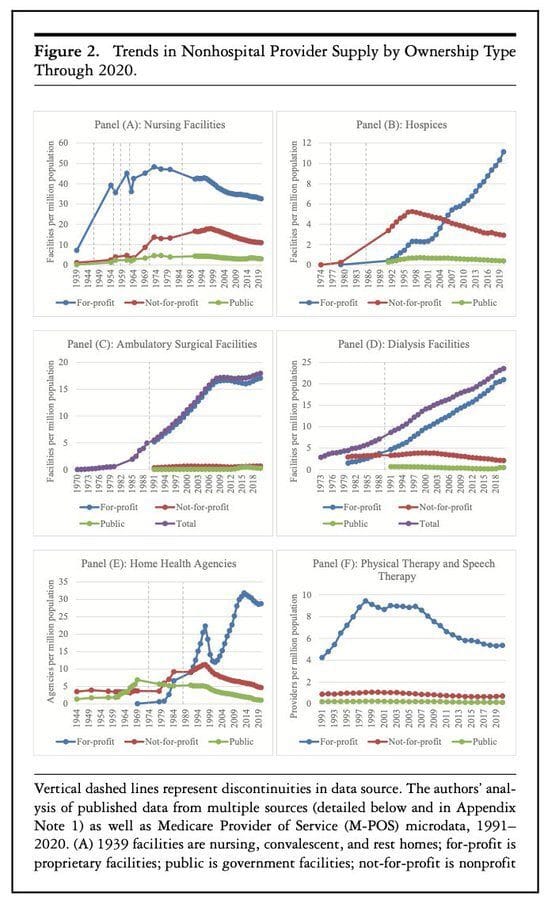
Milbank data on who owns healthcare delivery going back decades
It’s an interesting look back over the past century at how ownership of various parts of care delivery has changed. For many areas of care delivery highlighted in the chart below it’s not exactly a surprise to see for profit ownership taking off. But there’s some other interesting spaces where for profit investment peaked decades ago and has been declining since.