After the passage of the One Big Beautiful Bill Act (OBBBA), I found myself going back to one of my favorite essays, from Esquire Magazine of all places, called “Do We Really Want To Live Without The Post Office?” by Jesse Lichtenstein:
It’s expensive to get a letter to rural Mississippi and through the deep snow of the North Dakota plains and across the ocean to Martha’s Vineyard. It takes manpower, but also gas. Some areas are so sparsely populated that a postal route, public or private, may never turn a profit.
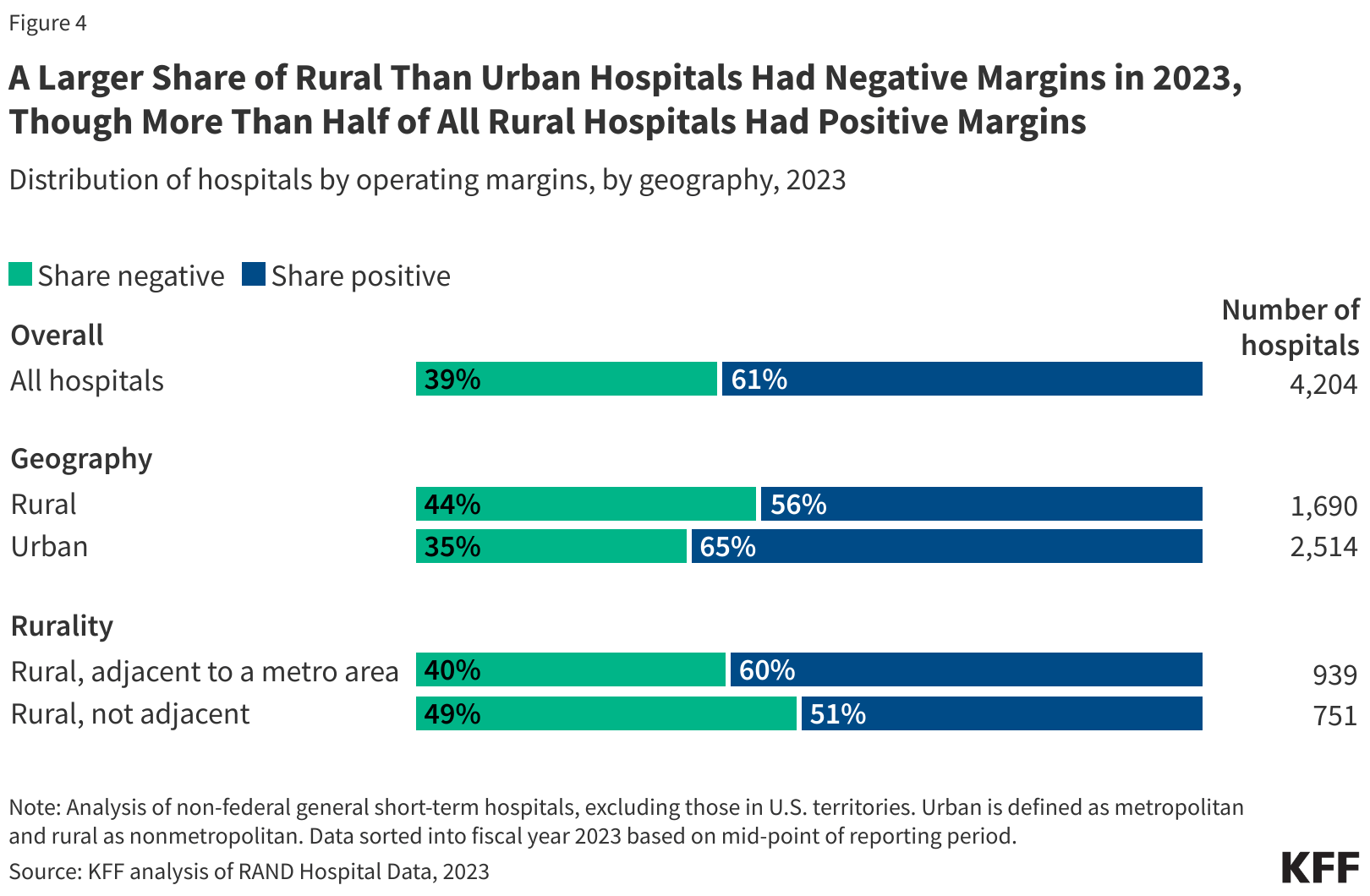
Although rural communities still have the benefit of the U.S. Postal Service, delivering rural healthcare poses similar sorts of challenges to delivering the mail in terms of logistics and unit economics. It’s harder and more expensive than delivering care in the city, and will only become more complicated and less profitable with the implementation of the OBBBA, which KFF estimates will cut federal Medicaid spending in rural areas by $137 billion. These cuts are being partially offset by the Rural Health Transformation Program’s $50 billion going to states with the goal of changing the math that makes the rural healthcare business so unforgiving.
Bracketing my skepticism about whether this sort of transformation is possible in the context of the enormous swing in funding, there are promising proof points out there like Hopscotch Primary Care which is building out a rural care model for seniors.
We hosted CEO Tim Gronniger and CMO Dr. Aditi Mallick live on HTN Discussions in late November, but they were also gracious enough to answer some more of our questions in a longer, written format, which I’m sharing here.
Questions
Q6: We spoke with Meera from Town Hall Ventures a few weeks back and she talked about Hopscotch as an example of how AI can enhance back-office and care delivery. Would love to hear about how you think about AI and any examples you can share about its business impact.
Interview
Q1: The conventional wisdom is that rural health is a hard business. From the outside, I would guess that the payer mix is worse, the labor market isn’t very favorable, and there is a higher prevalence of chronic diseases. On top of that, KFF estimates that under the One Big Beautiful Bill Act “federal Medicaid spending in rural areas could decrease by $137 billion over 10 years—about $87 billion more than is appropriated for the rural health fund.” Is this a reasonable accounting of the headwinds facing rural health? What’s the current state of primary care in rural America?
There are certainly headwinds in 2025, but to really understand the challenges facing rural health today, we believe it helps to zoom out and consider trends in rural health care over the past 25 years.
We see at least three key challenges:
Limited Access: Rural communities have 2X fewer physicians and 8X fewer specialists per capita than urban areas, with more than 700 rural hospitals at risk of closure.
Strained Infrastructure & Workforce: Rural communities face structural barriers across payers given broken fee-for-service economics, in addition to workforce challenges, highlighted by the fact that 25% of physicians in rural areas are projected to retire by 2030.
Large Burden of Chronic Disease: People living in rural America today are 40% more likely to have an avoidable hospitalization, 42% more likely to be readmitted, and 23% more likely to die from heart disease, cancer, or other leading causes of death. These disparities are only widening amid rising rates of chronic disease, depression, and economic hardship.
And on top of all that, fiscal pressures on Medicaid and other coverage sources that you mentioned continue to compound the challenge. So yes, the situation is difficult.
That said, there is also reason for optimism. Advances in technology make it possible to extend primary care and bring specialty services to rural America with a dramatically different footprint in cost & impact. Value-based care models are especially compelling in rural settings given the challenges with traditional fee-for-service economics and the heavier disease burden. The Rural Health Transformation Fund is a $50 billion transformation moment, an opportunity to reimagine rural care in a sustainable way. That’s exactly what we’ve been working toward at Hopscotch over the past four years.
Q2: Can you walk us through the Hopscotch business and what the economics of a “store” look like? What does your payer mix and patient population look like– MA, ACO, Medicaid Managed Care? In a typical value-based care arrangement, a big part of success is managing ER and hospital utilization– are those the same drivers in rural health or is there a different set of needs?
The first thing to note about our model is that we are solving the challenge of access head-on. We believe that the only way to make this work is to deliver high touch, high tech primary care in a way that energizes primary care teams.
Having spent years supporting primary care practices and managed services across both rural and urban geographies, we know that one of the hardest parts of operating in rural and small-town communities is connecting patients directly to providers and supportive care teams. For us, it starts with access!
But access alone isn’t enough. We’re also focused on providing the highest-quality care experience both in and out of the clinic, building longitudinal relationships with patients, ensuring consistent follow-up, closing care gaps, and managing chronic disease at a level that could stand alongside any top-tier urban care model.
When it comes to economics, payer mix, and patient population, our goal is to be the leading technology-enabled primary care provider for seniors in the country. We hold risk contracts with major Medicare payers in our founding market of Western North Carolina, aligning our incentives around driving improved outcomes.
On the utilization side, we see some familiar drivers around emergency room and hospital use. But in rural areas, those patterns are often amplified because the hospital is sometimes the default access point for most people. We’re changing that by offering 24/7, 365 primary care access, so patients have somewhere else to turn.
Beyond inpatient utilization, we’re also making it easier for patients to receive more comprehensive care in one place. We are expanding access to specialty care, either in-house or virtually, through partnerships or direct provision ourselves, which allows our PCPs to get a specialist consultation in under a minute, improving access and decreasing unnecessary utilization of specialty visits. We also offer in-house services such as labs, diabetic retinal eye exams, spirometry, and echocardiograms in-house. It’s been a meaningful win for both our patients and clinicians.
Ultimately, our model is designed to create a scalable, sustainable approach to rural primary care – one that expands access, aligns clinical excellence with economic viability, and delivers long-term impact for patients, clinicians, and communities.
Q3: Staffing, particularly physician staffing, is uniquely challenging for rural health organizations and primary care physicians are in high demand. Anecdotally, I’ve heard of doctors getting weekly outreach from staffing agencies to do work in rural areas, in some cases at 2x their normal rates. Can you walk me through the pitch to getting a primary care provider to take a job in a rural location today? How do you make the economic case to them? What is the pitch in its entirety beyond just the economic case?
Solving this challenge in a sustainable, scalable way is incredibly important. We’ve learned that the crisis in access to care in rural communities stems from a combination of workforce challenges.
the collapse of the independent, sole-proprietor practice model, and
the lack of viable practice opportunities that allow early- and mid-career physicians to practice in the way they want to practice.
The rural healthcare workforce is aging rapidly. Nearly 25% of rural providers plan to retire by 2030. We see this firsthand – physicians who have cared for their communities for decades, often serving thousands of patients, but who have no one to hand their practice to. And while many younger physicians express real interest in small town living – better work-life balance and lower cost of living, for example - they’re often discouraged by the administrative and financial challenges of running an independent practice – especially one that may lack modern technology and adequate support.
Our model directly addresses this structural challenge and offers a sustainable solution for both today’s and tomorrow’s workforce. We provide a natural succession pathway for physicians nearing retirement, while creating a modern, tech-forward, well-supported practice environment for early- and mid-career clinicians. By handling contracting, back-office operations, IT, HR, and other administrative burdens, hiring clinical support staff, and using workflow technology that empowers our care teams, we enable physicians to focus on what they do best – caring for patients. Further, our clinicians value the opportunity to truly know their patients, on both a medical and human level, because, by design, our model prioritizes outcomes and quality over the traditional fee-for-service focus on volume. Smaller patient panels and longer appointments mean PCPs can listen deeply, understand each patient’s story, and tailor care accordingly.
This approach creates a compelling value proposition for clinicians. In addition to competitive compensation and benefits, we can leverage significant public subsidies – often $100k or more in our communities – that will most likely double under new rural health transformation initiatives.
As a result, we’ve been able to recruit exceptional clinicians who deliver more personal, higher-quality care, which is strengthening both workforce stability and access in the communities that need it most.
Q4: My sense is that there are some returns to density and proximity in value-based care, but a big part of the story of rural health in America is hospital closures or reclassifications and fewer and fewer services being offered in these communities. How does Hopscotch think about specialty care and integrating with healthcare systems or providers that might be hours away?
We think of ourselves as a clinical hub – delivering care not just within our clinics, but also virtually and in patients’ homes. Our goal is simple: provide access to high-quality care where and when our patients need it.
When it comes to specialty care, access challenges are often amplified, with longer drive times and extended waits to see a specialist. Being able to provide or help coordinate access to specialty care is something we believe is incredibly valuable to our patients. A recent example illustrates this: a Hopscotch patient had been trying for months to schedule an appointment with an orthopedic specialist, without success. But the day after her Hopscotch visit, she received a call from the specialist’s office to set up an appointment. She credits the Hopscotch team for reaching out and coordinating on her behalf – turning what had been a frustrating, months-long process into a seamless, timely experience.
We also do this through partnerships that allow us to bring specialty care into our hubs, often in real-time during patient visits with virtual curbside consults, or "a specialist in your pocket". We have also developed strong relationships with the hospitals and health systems in the region who see our patients for procedures and planned admissions and then connect back to us through our Transitions of Care programs. This coordination ensures a smoother experience for our patients, supports timely follow-up that improves outcomes, and maintains continuity of care across the entire healthcare ecosystem.
Q5: When we first spoke, you talked about how important capitation is to make the math work. Capitation arrangements have been under pressure recently in MA plans. On the most recent earnings call, OptumHealth talked about 1% margins in their VBC arrangements. Would love to hear your thoughts on managing the transition from Fee For Service to VBC with Hopscotch clinics and doctors, especially in a time where there’s downward pressure from v28 and profitability challenges at the major payers?
While it’s true that value-based business models have faced pressure in recent years, especially with significant changes like V28 risk adjustment, there are a couple of points we’d like to underline.
First, Hopscotch has been succeeding in a post-V28 world. We began clinical operations in earnest in 2022 but only started taking risk contracts at meaningful scale in 2024 and 2025. We have been on the other side of V28 implementation consistently, and not only are we still standing, but we are doing exceptionally well. This is because we focus on delivering excellent care, building trust with patients, keeping them healthy, and managing costs effectively – not coding games.
Second, the challenges in managed care and at-risk provider businesses over the last few years are really part of a long-term cycle. If you broaden the lens, we see the best businesses and primary care groups have generally been built on the backbone of capitation and total responsibility for patient outcomes, utilization, and experience – this goes back decades, not four or five years.
Capitation economics allows for investment in innovation and technology to improve care and efficiency. In contrast, a fee for service model discourages innovation in efficiency in care delivery, as improvements are lost to time-based billing codes. Capitation, when paired with high-quality care, enables us to drive better care for patients and across the healthcare system.
Q6: We spoke with Meera from Town Hall Ventures a few weeks back and she talked about Hopscotch as an example of how AI can enhance back-office and care delivery. Would love to hear about how you think about AI and any examples you can share about its business impact.
We think of AI as supercharging human-centered care. When used effectively, it is a powerful force multiplier that both reduces administrative, back-office tasks and enhances care delivery. A few examples of how we’ve put this into practice and seen real impact include:
AI-Ambient Scribe: We have AI ambient scribes available in all our visits, including telehealth. Visit notes are transcribed in real time, and patients have clear, easy-to-understand visit summaries. The impact is immediate, and patients feel the difference - more eye contact and focused attention and clear after visit summaries so they don’t have to worry about capturing every detail. It’s a tool our care team truly embraces, with most of our PCPs using for more than 80% of appointments. Clinicians appreciate the smoother workflows, time saved (overall and after-hours), and accurate documentation that captures every detail. It’s a win-win for communication and care.
Revenue Cycle Management Enhancements: We partner with an AI-powered autonomous medical coding solution to streamline our RCM workflows, minimizing administrative burden and improving accuracy. These improvements not only optimize revenue cycle, but they are a big satisfier for our PCPs, as using AI for these tasks allows them to redirect valuable time and energy toward supporting our patients.
Point of Care Decision Support: We equip our PCPs with AI-powered clinical decision support tools that deliver concise, evidence-based answers at the point of care. By complementing clinicians’ knowledge, accelerating decision-making, and supporting patient education, it helps ensure every visit is informed and efficient. Used alongside Hopscotch’s guidelines and best practices, these tools allow our care teams to stay current, foster trust with patients, and deliver high-quality care, something both our care teams and patients consistently appreciate.
We are also exploring exciting partnerships that use AI to improve remote patient monitoring, longitudinal care management, upskilling of primary care providers, and real-time clinical decision support. With tech-enabled primary care, we can improve outcomes, ease clinicians’ workloads, and make communities healthier in a sustainable way.
Q7: We’ve heard from health systems that view the Rural Health Transformation Program as a tailwind, and are seemingly interested in acting as the “project managers” for managing rural health dollars in states. What role do you think large health systems will play in rural health over the coming years?
There is no doubt that health systems will continue to play an important role in care delivery in rural communities. They serve as the escalation pathway for acute care and the site of care for complex procedures and complicated cases. Their presence anchors local healthcare infrastructure and provides a vital safety net for communities that often have limited alternatives.
That said, it would be a mistake to assume that large health systems can or should shoulder this responsibility alone. Robust primary care in rural areas is a boon to health systems as it preserves space for high-acuity cases rather than filling Emergency Rooms and inpatient units with outpatient needs. From our experience, the best results come when primary care and health systems work as complementary partners, ensuring patients get the right care in the right place at the right time. This partnership is more sustainable, strengthens the local healthcare ecosystem, and ultimately delivers better outcomes for communities.
Q8: Geographically you're focused on North Carolina at the moment which has a number of things going for it– a forward -thinking healthcare policy makers at the state level, state subsidies to help recruit doctors, a beautiful landscape. How are you thinking about expansion? What makes a state attractive to Hopscotch? If a state was thinking about spending Rural Health Transformation Program dollars on something to make it more attractive to Hopscotch, what would those investments look like?
We love serving communities in North Carolina, and we’re excited to bring this model to millions of seniors in small towns and rural communities across the country.
When evaluating new markets, we focus on several key parameters:
Primary Care Supply vs. Demand Imbalance: Is there significant primary care supply vs. demand imbalance – particularly with high-needs populations like those covered by Medicare and Medicaid? It’s not difficult to identify rural communities that would benefit from additional, sustainable care capacity – unfortunately, this is the norm.
Payer Landscape: Are there payer partners who share our vision for improving access and outcomes through primary care and have experience with value-based contracting? Again, most payers struggle to serve rural regions, so we have found great interest in our model among payers.
Workforce Training Infrastructure: Are there strong medical schools and healthcare workforce training organizations (both private and public) within the state that we can tap into – particularly those that are focused on rural areas?
We are especially eager to collaborate with states interested in using RHTP funds to support one-time start-up costs helping to build sustainable, high-quality primary care for rural communities nationwide. CMS has prioritized sustainability of RHT initiatives, so our approach, which requires no public funding beyond the period of the Transformation Fund, while providing ongoing access to top-tier primary care, is well-suited to the moment.
